Executive Summary
In an effort to better understand how physicians feel about their jobs, including their workload and communication with patients and the correlation between mental health and workload, locumstory.com surveyed more than 3,700 physicians in nearly every specialty, work setting and region of the country.
In 2016, locumstory.com conducted a similar study. This year’s survey examines changes over the past two years in physicians’ sentiments about their profession. The good news is that physicians in 2018 feel less overworked than they did two years ago. This doesn’t mean overwork isn’t an issue, but it appears to be moving in a positive direction. However, physicians are still faced with burnout, mental health issues and not enough time with patients.
Burnout is someone else’s problem
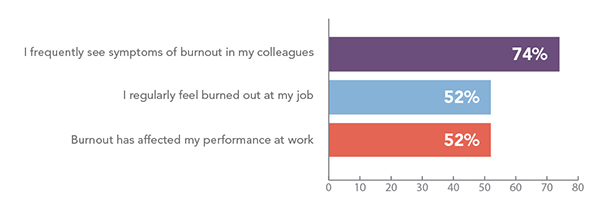
Physician burnout has been a trending topic for years but physicians don’t always recognize it within themselves. Though 74 percent of physicians reported frequently seeing symptoms of burnout in others, only 52 percent of them reported regularly feeling burned out themselves.
The most common burnout symptoms physicians experience are irritability and apathy, and about half of physicians also experience chronic fatigue and impaired memory and attention.
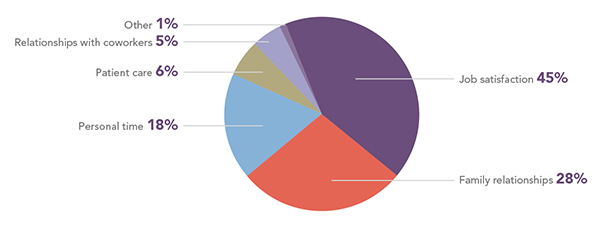
What does burnout impact the most? Forty percent of physicians cite job satisfaction; more than a quarter say family relationships.
Workload affects physician mental health and thoughts of suicide
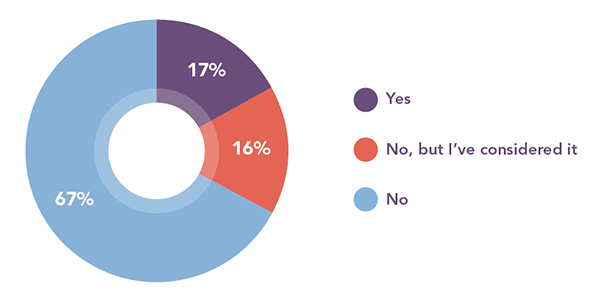
More than half of physicians (51 percent) reported that their workload had impacted their mental health, but only 17 percent have sought help and two-thirds say they would not consider meeting with a mental health professional at all. This is likely due to 53 percent of physicians feeling mental health is a taboo topic to discuss. While some (23 percent) have access to mental healthcare through work, most don’t. Of those who do not have access to mental healthcare, 45 percent would like it and 55 percent would not.
Six percent of physicians have contemplated suicide because of the demands of their profession and 11 percent take medication for anxiety or depression. Most of the physicians who take medication say that their profession contributes to their anxiety or depression.
Workloads are heavy, but improving
More than half of physicians (55 percent) have less free time outside of work than when they first started their career. However, these numbers have improved in the past two years. When asked the same question in 2016, 64 percent of physicians reported having less free time.
Physicians are also feeling more overworked now than when they first started practicing. However, like free-time, these numbers have improved since the 2016 survey. Today, just 56 percent of physicians feel overworked compared to 65 percent two years ago.
Additionally, the number of physicians considering leaving their profession prior to age 65 has dropped by 2 percent since 2016. However, more than half of physicians still considered leaving the profession early due to workload.
Time spent with patients is improving
Overall, most physicians feel they spend less time with patients now than when they started their careers and almost all want more direct time with patients. However, these numbers have also improved. In 2016, 58 percent of physicians said they were spending less time patients than they used to, compared to 46 percent today.
Survey Report
Physician burnout
Physician burnout has been a trending topic for years, but physicians don’t always recognize it within themselves. Though 74 percent of physicians reported frequently seeing symptoms of burnout in others, only 52 percent of them reported regularly feeling burned out themselves.
Do you see burnout in yourself or others?
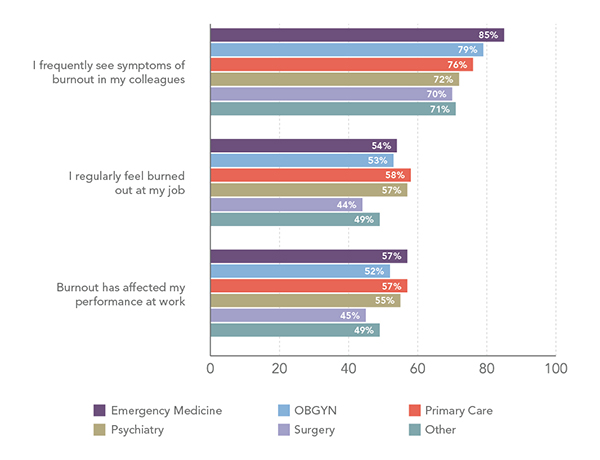
Surgeons are significantly less likely to self-report burnout than physicians in emergency medicine, OBGYN, primary care, and psychiatry.
Physicians in emergency medicine are significantly more likely to observe burnout in their colleagues than those in primary care, psychiatry, surgery, and other specialties.
Burnout and burnout observation, by specialty
The most common burnout symptoms physicians experience are related to their attitudes and emotions — particularly irritability and apathy. About half of physicians also experience chronic fatigue and impaired memory and attention.
What are the symptoms and signs of your burnout?
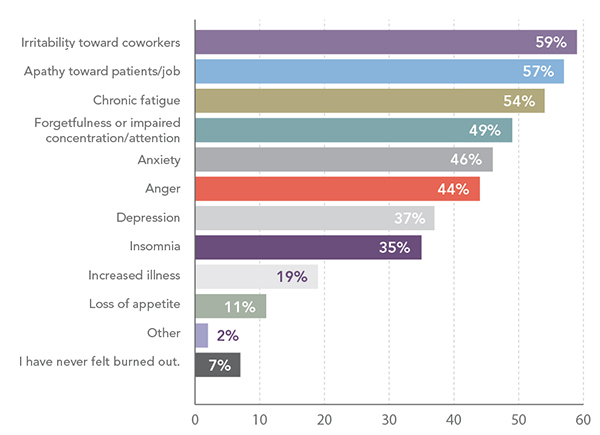
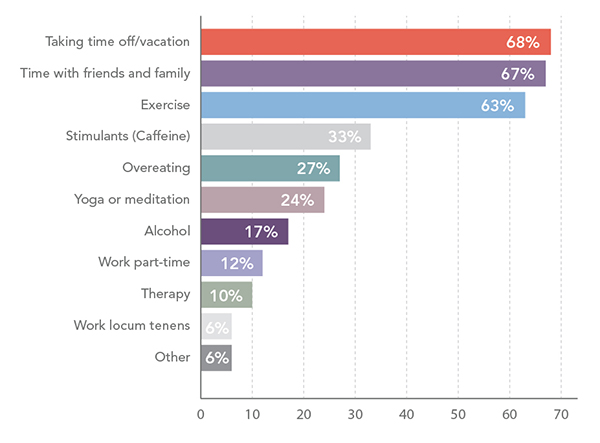
Forty percent of physicians say their job satisfaction suffers the most from burnout. More than a quarter say family relationships suffer. To cope, two-thirds of physicians take time off or spend time with loved ones, and more than half exercise.
Life aspects that suffer the most due to burnout
Methods for coping with burnout
Workload affects physician mental health
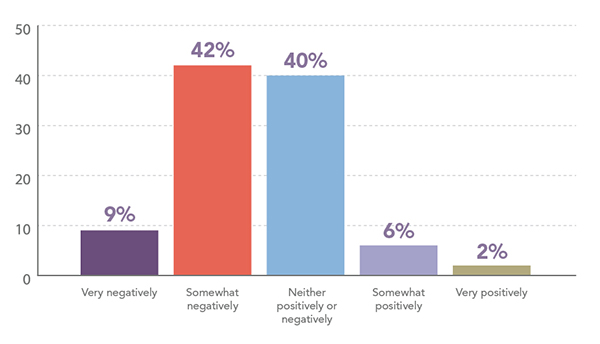
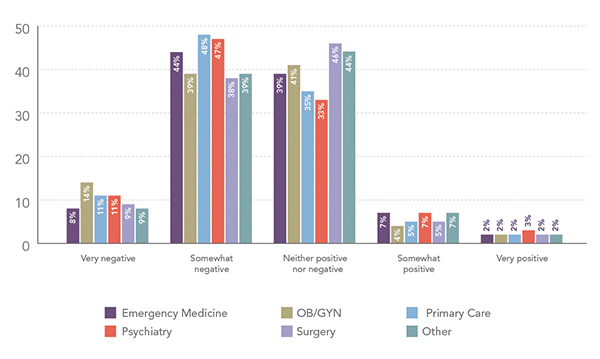
While more than half of physicians’ workload (51 percent) has impacted their mental health, only 17 percent have sought help and two-thirds say they would not consider meeting with a mental health professional. Physicians in primary care (59 percent) and psychiatry (58 percent) are more likely to say their workload negatively impacts their mental health than physicians in other specialties.
Impact of workload on mental health
Impact of workload on mental health, by specialty
Have you ever met with a mental health professional?
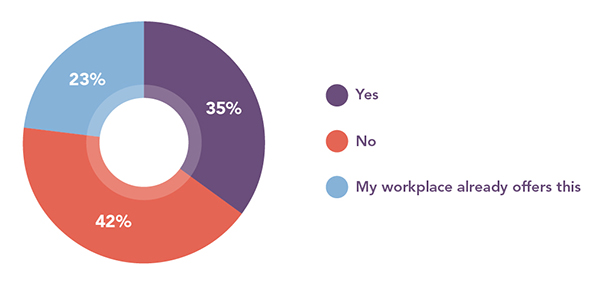
More than half of physicians (53 percent) feel mental health is a taboo topic to discuss. And while some (23 percent) have access to mental healthcare through work, most don’t. Of those who do not have access to mental healthcare 45 percent would like it and 55 percent would not.
While more than a third would like workplace access to a mental health professional, even more would not. Physicians in primary care are the least likely to say mental health is taboo, even compared to those in psychiatry.
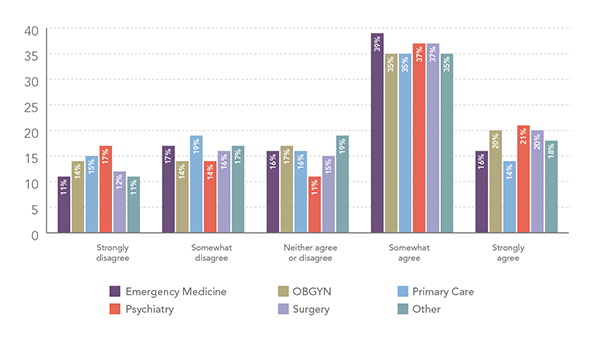
Mental health is a taboo topic
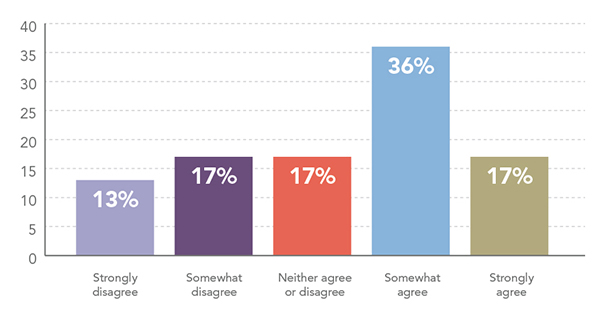
Mental health is a taboo topic, by specialty
Do you want workplace access to a mental health professional?
Six percent of physicians have contemplated suicide because of their profession. Eleven percent take medication for anxiety or depression. Most of the physicians who take medication (85 percent) say that their profession contributes to their anxiety or depression. Physicians in OBGYN and psychiatry are significantly more likely to take medication for anxiety or depression than physicians in other specialties.
Physical health also impacts the way physicians practice. Eighty-three percent of physicians reported having gone to work sick and 37 percent say burnout contributes to their being ill.
Physician workload
More than half of physicians have less free time outside of work than when they first started their career. However, these numbers have improved in the past two years. When asked the same question in 2016, 64 percent of physicians reported having less free time.
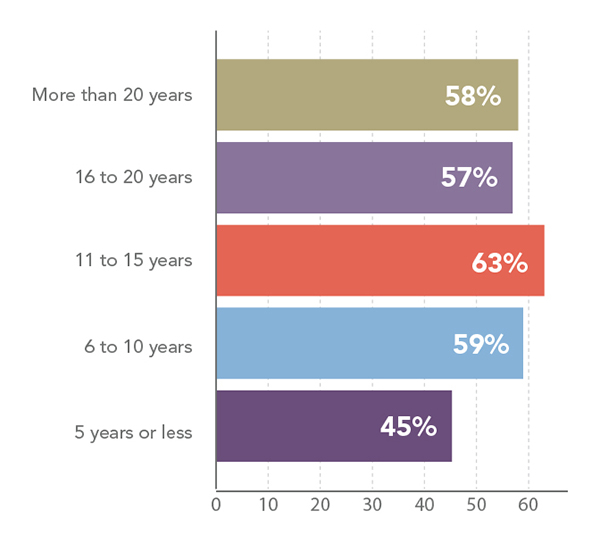
Physicians who have been in the field for more than five years are significantly more likely to have less free time now than when they first began practicing, compared to those who have five years of experience or less. Those practicing for 11 to 15 years have the least perceived free time of any other age group, even those with more than 16 years of experience.
How much free time do you have, compared to when you began your career?
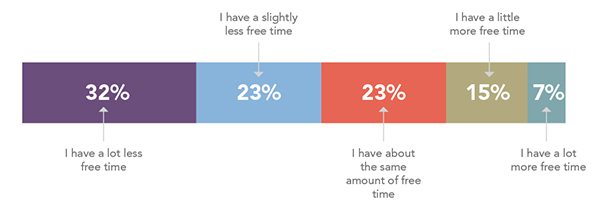
Physicians are less likely to report they have less free time (55%) than in 2016 (64%).
Physicians reporting less free time, by years of practice
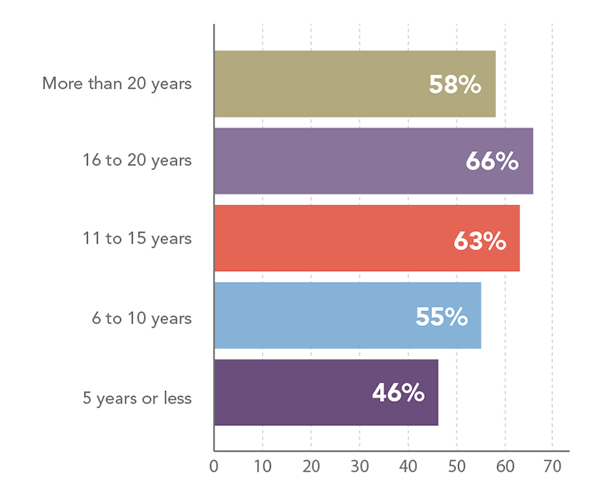
Physicians are also feeling more overworked now than when they first started practicing. Physicians with more than five years of experience are significantly more likely to feel more overworked than those with less experience. However, like free-time, these numbers have improved since the 2016 survey. Today, just 56 percent of physicians feel overworked compared to 65 percent two years ago.
Physician work
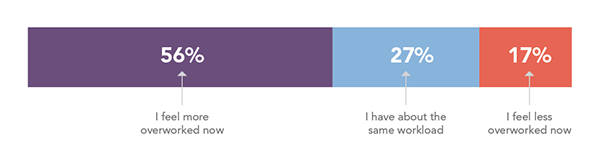
Physicians are significantly less likely to feel more overworked in 2018 (56%) than in 2016 (65%).
Overwork, by years of experience
Physicians’ thoughts on work/life balance in their facilities is almost evenly split with 41 percent thinking their facility supports a healthy work/life balance and 39 percent feeling it does not. These numbers have also improved since 2016 when only 35 percent felt their facility offered healthy work/life balance.
Facility supports a healthy work/life balance
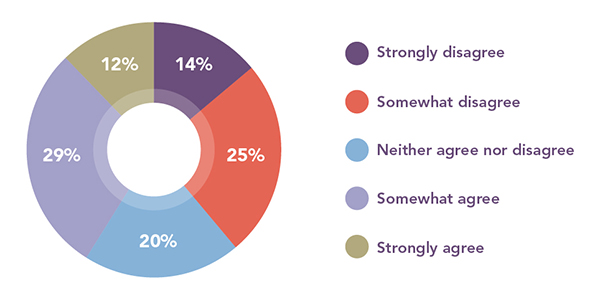
More physicians agree their facility supports work/life balance (41%) than in 2016 (35%).
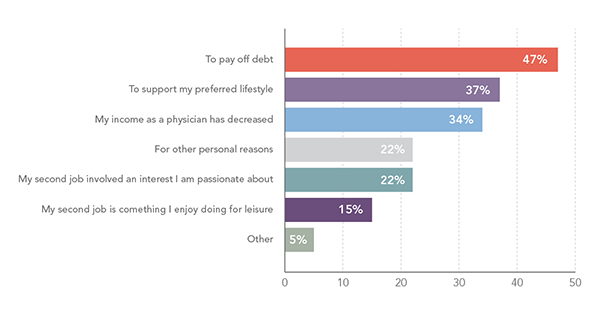
Sixty percent of physicians reported taking additional jobs to supplement their income. Of those, half have taken additional jobs to pay off debt. Physicians are much less likely to take an additional job for personal or leisure reasons. The top three reasons for extra work — to pay off debt, to support a preferred lifestyle and because their income had decreased — were the same top three answers in 2016, although paying off debt is now higher and decreased income is lower.
Reasons physicians work a second job
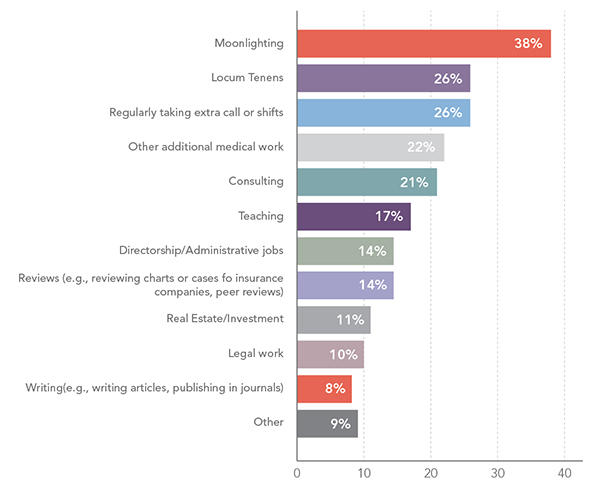
For those who do work second jobs the top job is moonlighting, followed by locum tenens and taking on extra shifts or call. The “other” category includes such interesting jobs as ringside physician for combat sports, motivational speaking, Uber driver, and working as a DJ.
Where physicians are finding second jobs
More than half of physicians considered leaving their profession within the past few years (53 percent), similar to what was found in 2016 (55 percent). More than half of physicians have considered quitting because they spend too much time entering data into electronic health records, feel overworked, or spend too much time on paperwork. Physicians in emergency medicine are more likely to consider quitting before retirement age than physicians who work in other specialties.
Why physicians have thought about quitting medicine prior to retirement age
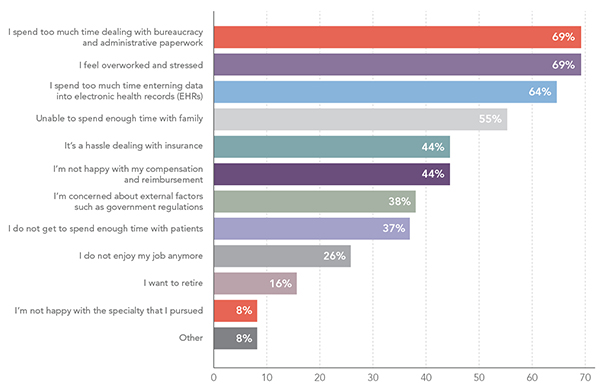
Top 3 Reasons in 2016:
1. Too much time on EHR data entry: 68%
2. Overworked: 62%
3. Too much time on paperwork: 59%
Workplace perceptions
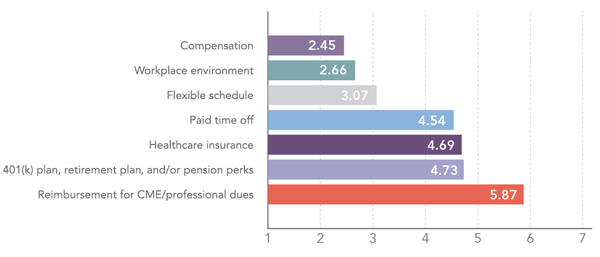
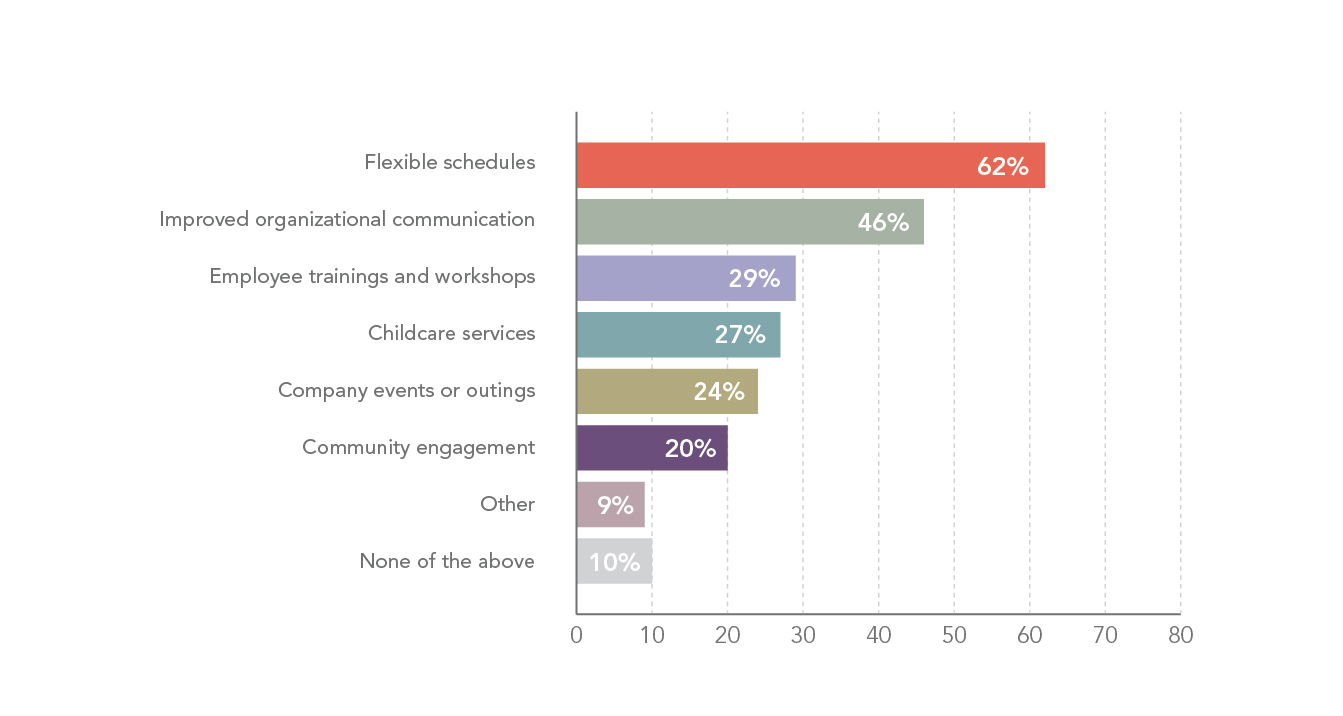
Physicians value compensation the most in the workplace, followed by work environment and a flexible schedule. Almost two-thirds (62 percent) of physicians say flexible schedules would improve workplace culture. Almost half think improved organizational communication would also improve work culture.
What is valued most in a workplace? Based on a 1 (most valuable) to 7 (least valuable) scale
What improves a workplace culture?
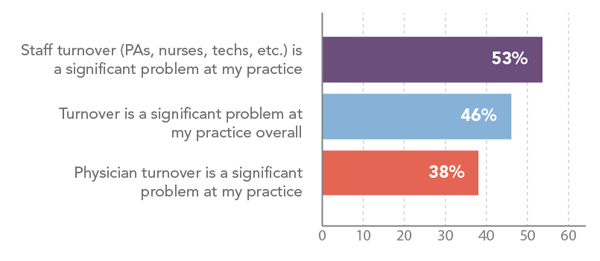
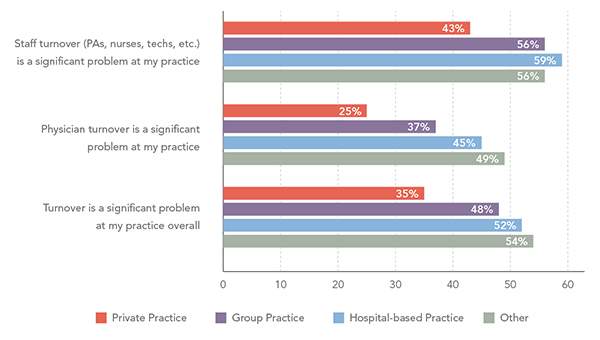
About half of physicians believe that staff and overall turnover is a problem at their practice. Private practice physicians have the least issues with turnover. Hospital-based physicians have the most problems with turnover.
Turnover issues
Turnover issues, by practice setting
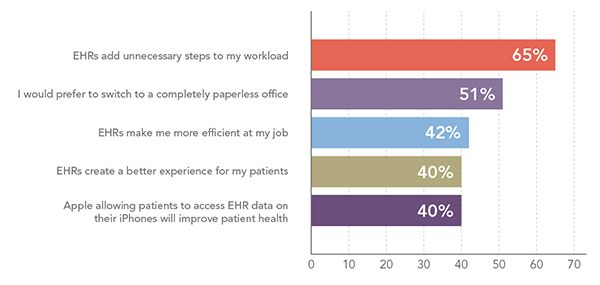
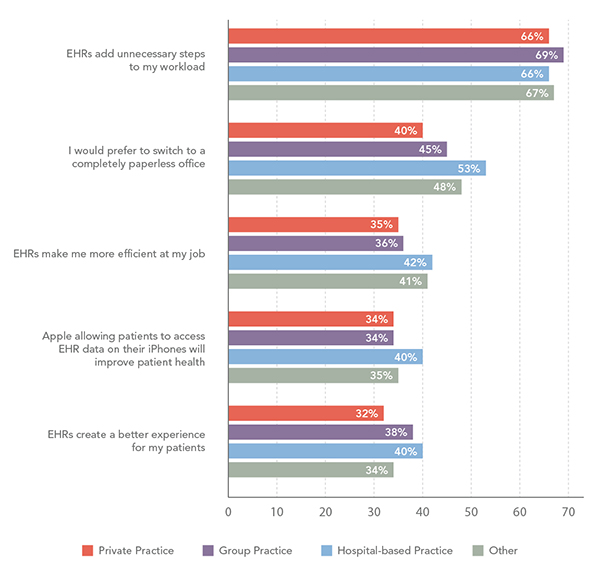
Regardless of practice setting, almost two-thirds of physicians agree that EHRs add unnecessary steps to their workload. Physicians working in private practice are significantly less likely to prefer switching to a paperless office than physicians in hospital-based and other practice settings.
Physicians thoughts on Electronic Health Records (EHRs)
EHR thoughts, by practice setting
Patient time
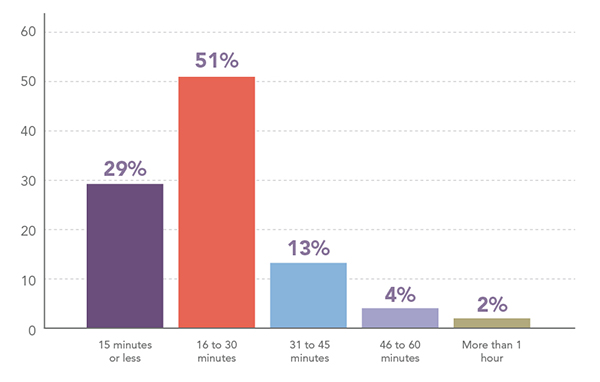
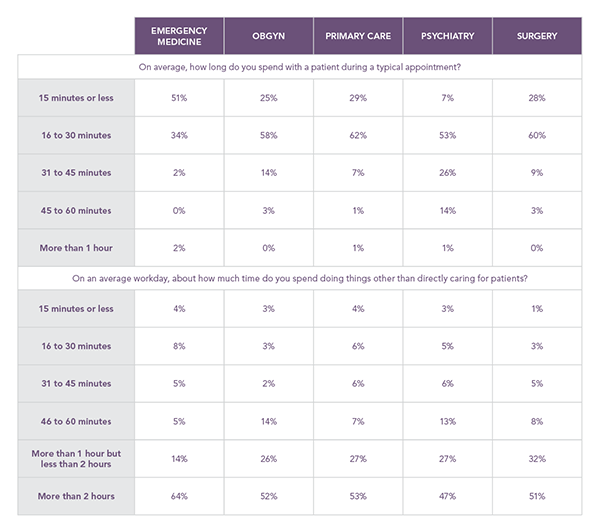
The average patient appointment takes 30 minutes or less but 25 percent of physicians spend more than one hour a day on indirect patient tasks, such as charting, billing and paperwork. Half of physicians spend more than two hours on these tasks each day.
Average time spent with a patient
Average time spent on paperwork per day
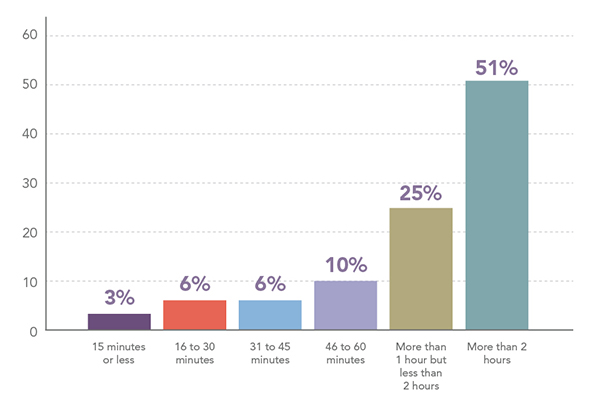
Patient and paperwork time are fairly consistent across medical specialties with one exception. Physicians in emergency medicine are significantly more likely to spend 15 minutes or less with patients than physicians in all of the other specialties, likely due to the pressing nature of the visits. However, they spend more time on paperwork than other specialties.
Time spent with patients, by specialty
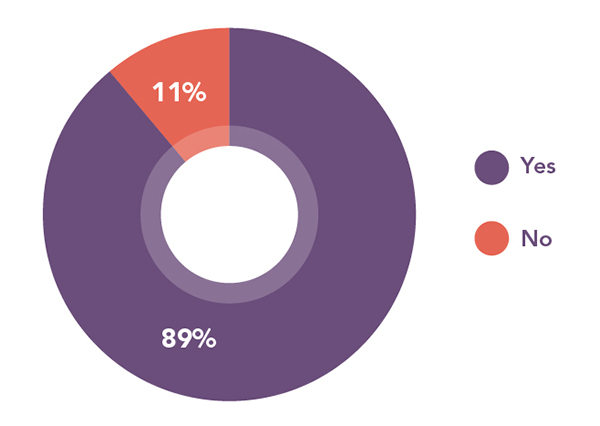
Overall, most physicians feel they spend less time with patients now than when they started their careers and almost all want more direct time with patients. However, these numbers have improved. In 2016, 58 percent of physicians said they were spending less time patients than they used to, compared to 46 percent today.
Time spent with patients compared to when you started your career
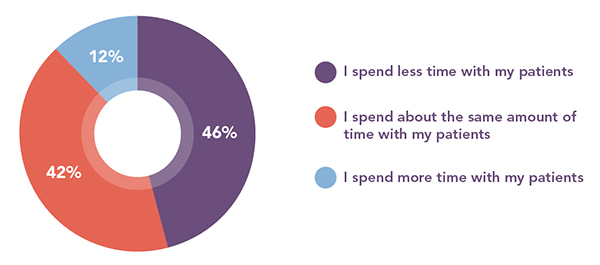
Physicians are significantly less likely to say they spend less time with their patients (46%) now than in 2016 (58%).
Do you want more time with patients?
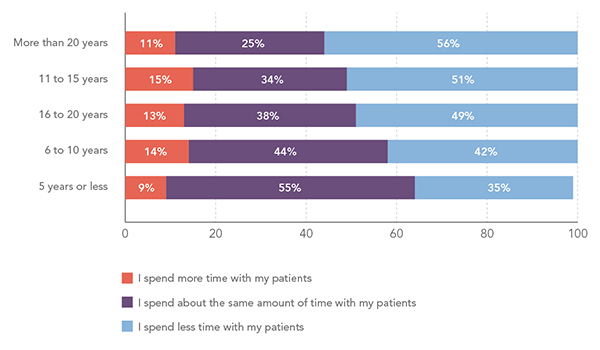
There is a correlation between time spent with patients and how long a physician has been working. The longer a physician practices, the less time they spend with patients.
Patient time by years in practice
Communication
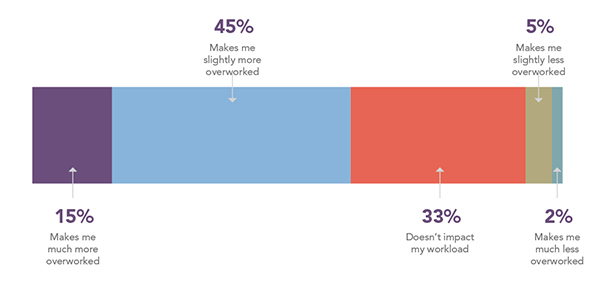
More than three-quarters of physicians communicate with patients outside work. Nearly half of those physicians are spending one to three hours communicating with patients. Of those who spend time communicating outside work, 60 percent say it makes them at least slightly overworked.
Time spent communicating with patients outside of work
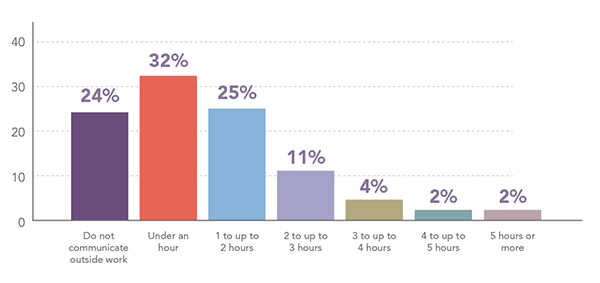
The impact of after-hours communication on workload
Most physicians offer communication by phone and more than half use email/messaging through a patient portal. Text messaging, social media and video messaging are the least offered, and physicians are least interested in offering these methods of communication to patients. Since 2016, use of patient portals has increased from 46 percent to 57 percent and there has been a 31 percent increase in interest in telemedicine.
Patient communication tools
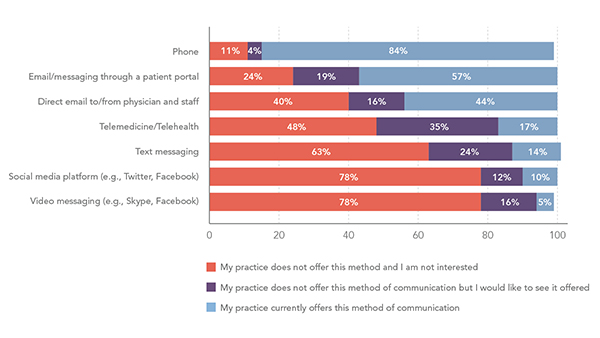
Physicians are significantly more likely to use patient portals in 2018 (57%) than in 2016 (46%). There is also more interest in telemedicine in 2018 (35%) than in 2016 (4%).
Methodology
Locumstory.com surveyed 3,753 actively practicing physicians in a large variety of specialties from around the country. The goal of the study was to better understand the role of physicians and their day-to-day job activities, specifically looking at workload, mental health, and burnout. Locumstory.com is a site dedicated to sharing physicians’ stories of working locum tenens and general locum tenens knowledge. Learn more at locumstory.com.
Download a PDF of the survey report.

